Lawmakers Hear Calls to Treat Youth Violence as a Public‑Health Emergency in U.S. Virgin Islands Hearing
October 31, 2025 | 2025 Legislature, Virgin Islands
This article was created by AI summarizing key points discussed. AI makes mistakes, so for full details and context, please refer to the video of the full meeting. Please report any errors so we can fix them. Report an error »
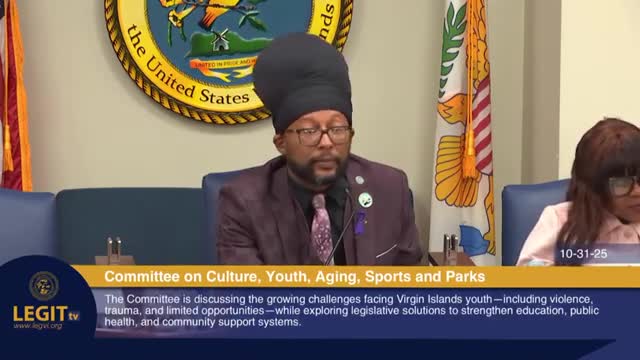
Senators heard a series of testimonies on Oct. 31, 2025, urging the Legislature to treat youth violence as a public‑health problem and to shore up behavioral‑health capacity, data sharing and stable funding for community programs.
Dr. Nicole Cragwell Sims, acting commissioner of the Virgin Islands Department of Health, said local and national surveys show high levels of emotional distress and risky behavior among youth and argued that the territory needs trauma‑informed, culturally grounded services. "The Department of Health views youth violence not merely as a criminal or social issue, but as a symptom of a deeper trauma and unaddressed behavioral health need that demands a coordinated trauma informed response," Dr. Sims said, outlining mobile crisis teams, a Zen‑van outreach effort and a federally funded Zen‑room school pilot as current efforts.
Antonio Emmanuel, executive director of the Office of Gun Violence Prevention, described a team of community engagement coordinators, violence interrupters and survivor‑engagement specialists who have worked in schools and neighborhoods and who have delivered anti‑bullying and violence prevention sessions to thousands of students. "The Office of Gun Violence Prevention is managing gun violence as a health epidemic and encouraging mindset change," Emmanuel said.
The Virgin Islands Police Department, represented by Sergeant Danisha Samuel Santos, described diversion and crisis‑intervention practices the department has adopted in juvenile and school settings. "Our mission extends beyond enforcement to encompass prevention, intervention, and collaboration with our partners in education, behavioral health, human services, and community service organizations," Sergeant Santos said, while noting that officer staffing and interagency coordination remain constraints.
Attorney General Gordon Rhea and Assistant Attorney General Chad Mitchell highlighted juvenile caseloads, recidivism and gaps in rehabilitative services. Mitchell said repeat offending is often driven by a lack of real economic and training opportunities and urged more vocational pathways and mentorships for justice‑involved youth. "We need to really engage them with that thought process of what am I going to do with my life, and how do I get there?" Mitchell said.
Community providers described on‑the‑ground programs and funding shortfalls. Karita Stevens Gumbs of the Village Partners in Recovery outlined prevention and adolescent treatment programs, including ARC outpatient services that have reached hundreds of youth but face an uncertain funding horizon when federal grants end. Christie Payne of My Brother’s Workshop described vocational training, diplomas and certifications and said general appropriations to her nonprofit had fallen sharply, forcing reliance on earned revenue and reserves.
Diana James of the Saint Croix Foundation (Kids Count USVI) urged lawmakers to translate data into coordinated funding and policy. She highlighted enduring child poverty (33 percent territorywide in 2020; 42 percent for children under 5 in St. Croix) and mental‑health indicators from the territory’s Youth Risk Behavior Survey.
Committee members pressed witnesses on the size of the behavioral‑health workforce. Director Giselle Ramos (DOH behavioral health) said clinicians are limited: four full‑time clinicians in St. Thomas, one full‑time clinician in St. Croix, and two part‑time psychiatrists with cross‑island coverage. DOH estimated it needs several more clinicians, outreach workers and case managers across the islands and agreed to provide a written staffing breakdown to the committee.
Senators and witnesses repeatedly called for better data sharing and cross‑agency protocols so that schools, law enforcement, health and social services can coordinate crisis response and follow‑up care. Nonprofits urged predictable local funding to sustain programs now supported by time‑limited federal grants.
The committee did not take formal votes during the hearing. Multiple agencies pledged follow‑up materials: DOH said it would send a staffing plan; nonprofits offered program cost details; the Saint Croix Foundation and Bureau of Economic Research described ongoing work to assemble administrative data and public dashboards. The committee signaled it will continue the conversation to translate testimony into specific proposals.
For readers: key existing services referenced in testimony include DOH behavioral‑health outreach and a Zen‑room pilot for schools, OGVP community engagement and violence interrupter teams, VIPD diversion and school‑resource efforts, the 988 suicide/crisis lifeline (national network with territory activation), and community programs such as ARC and My Brother’s Workshop.
Dr. Nicole Cragwell Sims, acting commissioner of the Virgin Islands Department of Health, said local and national surveys show high levels of emotional distress and risky behavior among youth and argued that the territory needs trauma‑informed, culturally grounded services. "The Department of Health views youth violence not merely as a criminal or social issue, but as a symptom of a deeper trauma and unaddressed behavioral health need that demands a coordinated trauma informed response," Dr. Sims said, outlining mobile crisis teams, a Zen‑van outreach effort and a federally funded Zen‑room school pilot as current efforts.
Antonio Emmanuel, executive director of the Office of Gun Violence Prevention, described a team of community engagement coordinators, violence interrupters and survivor‑engagement specialists who have worked in schools and neighborhoods and who have delivered anti‑bullying and violence prevention sessions to thousands of students. "The Office of Gun Violence Prevention is managing gun violence as a health epidemic and encouraging mindset change," Emmanuel said.
The Virgin Islands Police Department, represented by Sergeant Danisha Samuel Santos, described diversion and crisis‑intervention practices the department has adopted in juvenile and school settings. "Our mission extends beyond enforcement to encompass prevention, intervention, and collaboration with our partners in education, behavioral health, human services, and community service organizations," Sergeant Santos said, while noting that officer staffing and interagency coordination remain constraints.
Attorney General Gordon Rhea and Assistant Attorney General Chad Mitchell highlighted juvenile caseloads, recidivism and gaps in rehabilitative services. Mitchell said repeat offending is often driven by a lack of real economic and training opportunities and urged more vocational pathways and mentorships for justice‑involved youth. "We need to really engage them with that thought process of what am I going to do with my life, and how do I get there?" Mitchell said.
Community providers described on‑the‑ground programs and funding shortfalls. Karita Stevens Gumbs of the Village Partners in Recovery outlined prevention and adolescent treatment programs, including ARC outpatient services that have reached hundreds of youth but face an uncertain funding horizon when federal grants end. Christie Payne of My Brother’s Workshop described vocational training, diplomas and certifications and said general appropriations to her nonprofit had fallen sharply, forcing reliance on earned revenue and reserves.
Diana James of the Saint Croix Foundation (Kids Count USVI) urged lawmakers to translate data into coordinated funding and policy. She highlighted enduring child poverty (33 percent territorywide in 2020; 42 percent for children under 5 in St. Croix) and mental‑health indicators from the territory’s Youth Risk Behavior Survey.
Committee members pressed witnesses on the size of the behavioral‑health workforce. Director Giselle Ramos (DOH behavioral health) said clinicians are limited: four full‑time clinicians in St. Thomas, one full‑time clinician in St. Croix, and two part‑time psychiatrists with cross‑island coverage. DOH estimated it needs several more clinicians, outreach workers and case managers across the islands and agreed to provide a written staffing breakdown to the committee.
Senators and witnesses repeatedly called for better data sharing and cross‑agency protocols so that schools, law enforcement, health and social services can coordinate crisis response and follow‑up care. Nonprofits urged predictable local funding to sustain programs now supported by time‑limited federal grants.
The committee did not take formal votes during the hearing. Multiple agencies pledged follow‑up materials: DOH said it would send a staffing plan; nonprofits offered program cost details; the Saint Croix Foundation and Bureau of Economic Research described ongoing work to assemble administrative data and public dashboards. The committee signaled it will continue the conversation to translate testimony into specific proposals.
For readers: key existing services referenced in testimony include DOH behavioral‑health outreach and a Zen‑room pilot for schools, OGVP community engagement and violence interrupter teams, VIPD diversion and school‑resource efforts, the 988 suicide/crisis lifeline (national network with territory activation), and community programs such as ARC and My Brother’s Workshop.
View the Full Meeting & All Its Details
This article offers just a summary. Unlock complete video, transcripts, and insights as a Founder Member.
✓
Watch full, unedited meeting videos
✓
Search every word spoken in unlimited transcripts
✓
AI summaries & real-time alerts (all government levels)
✓
Permanent access to expanding government content
30-day money-back guarantee
