OCA Proposes New Framework for Behavioral Health Spending Allocation
July 26, 2025 | Department of Health Care Access and Information, Agencies under Office of the Governor, Executive, California
This article was created by AI summarizing key points discussed. AI makes mistakes, so for full details and context, please refer to the video of the full meeting. Please report any errors so we can fix them. Report an error »
The recent meeting of the OHCA Investment and Payment Workgroup, held on July 26, 2025, focused on the allocation of non-claim spending in behavioral health, a critical area of concern for California's healthcare system. The discussions centered around the recommendations made by the Office of Care Access (OCA) regarding how to categorize and measure behavioral health spending effectively.
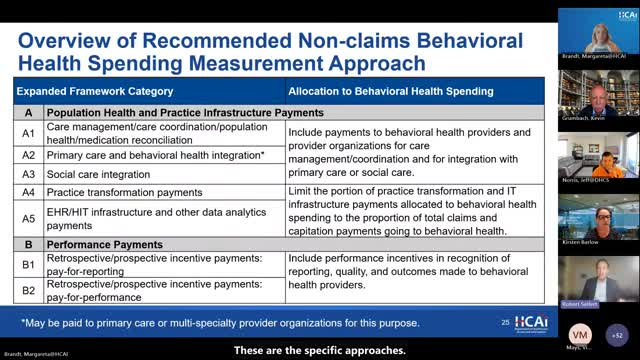
A significant portion of the meeting was dedicated to outlining the expanded framework's subcategories for allocating non-claim spending. The OCA proposed that payments made to behavioral health providers and organizations should be classified as behavioral health spending, particularly under the framework's categories A, B, C, D, and E. This classification is essential for ensuring that funding is directed appropriately to support behavioral health services.
In category A, the OCA emphasized that payments for primary care and behavioral health integration would be included in the behavioral health spending measurement. The recommendation also included a limit on spending in certain subcategories, which would be proportional to the overall claims and capitation payments allocated to behavioral health. This approach aims to ensure that the funding reflects the actual spending on behavioral health care.
The meeting also addressed performance payments in category B, which would be recognized as behavioral health payments when directed to relevant providers. Additionally, category C discussed shared savings arrangements, noting that condition-related episode-based payments would count towards behavioral health spending if they pertain to behavioral health care.
Categories D and E focused on capitation payments, with the OCA recommending that 100% of behavioral health capitation payments be included in the measurement of behavioral health spending. The allocation for more general capitation payments would follow a similar formula used for primary care, ensuring consistency in how funds are distributed.
The workgroup paused for comments and questions, inviting further input from participants to refine the recommendations. The discussions highlighted the ongoing efforts to enhance the funding structure for behavioral health services in California, reflecting a commitment to improving care access and quality for individuals in need.
As the meeting concluded, the OCA encouraged participants to share any additional thoughts or suggestions post-meeting, indicating a collaborative approach to finalizing the recommendations. The outcomes of this meeting are expected to play a crucial role in shaping the future of behavioral health funding and service delivery in the state.
A significant portion of the meeting was dedicated to outlining the expanded framework's subcategories for allocating non-claim spending. The OCA proposed that payments made to behavioral health providers and organizations should be classified as behavioral health spending, particularly under the framework's categories A, B, C, D, and E. This classification is essential for ensuring that funding is directed appropriately to support behavioral health services.
In category A, the OCA emphasized that payments for primary care and behavioral health integration would be included in the behavioral health spending measurement. The recommendation also included a limit on spending in certain subcategories, which would be proportional to the overall claims and capitation payments allocated to behavioral health. This approach aims to ensure that the funding reflects the actual spending on behavioral health care.
The meeting also addressed performance payments in category B, which would be recognized as behavioral health payments when directed to relevant providers. Additionally, category C discussed shared savings arrangements, noting that condition-related episode-based payments would count towards behavioral health spending if they pertain to behavioral health care.
Categories D and E focused on capitation payments, with the OCA recommending that 100% of behavioral health capitation payments be included in the measurement of behavioral health spending. The allocation for more general capitation payments would follow a similar formula used for primary care, ensuring consistency in how funds are distributed.
The workgroup paused for comments and questions, inviting further input from participants to refine the recommendations. The discussions highlighted the ongoing efforts to enhance the funding structure for behavioral health services in California, reflecting a commitment to improving care access and quality for individuals in need.
As the meeting concluded, the OCA encouraged participants to share any additional thoughts or suggestions post-meeting, indicating a collaborative approach to finalizing the recommendations. The outcomes of this meeting are expected to play a crucial role in shaping the future of behavioral health funding and service delivery in the state.
View full meeting
This article is based on a recent meeting—watch the full video and explore the complete transcript for deeper insights into the discussion.
View full meeting
